A recent study published in the Journal of Internal Medicine has uncovered a connection between severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, the virus responsible for the coronavirus disease 2019 (COVID-19), and the development of complications in benign prostatic hyperplasia (BPH).
The study investigated the possibility that SARS-CoV-2 could infect the lower urinary tract in males, as the prostate epithelial cells express both angiotensin-converting enzyme 2 (ACE2) and transmembrane protease serine 2 (TMPRSS2), which are receptors for the virus. It was hypothesized that COVID-19 could have an impact on BPH, as metabolic syndrome and diabetes mellitus, both risk factors for lower urinary tract symptoms (LUTS), are known to be associated with COVID-19.
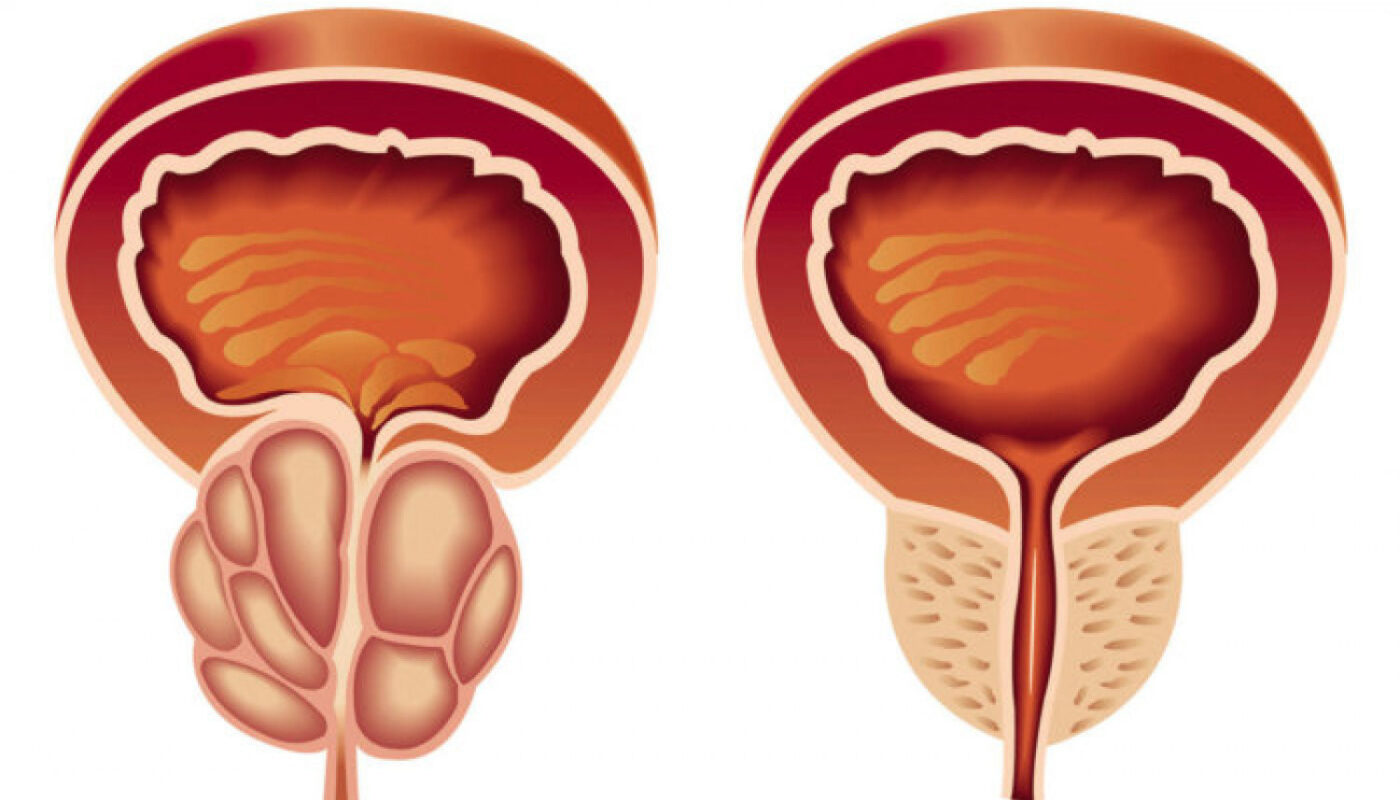
BPH can lead to complications such as urinary tract infections (UTIs), retention of urine (ROU), bladder stones, and hematuria. COVID-19 and BPH are both more prevalent in older males, which raises the possibility that COVID-19 patients may be at a higher risk of developing complications related to BPH. However, there is limited existing evidence on the relationship between COVID-19 and LUTS.
To investigate this further, researchers analyzed relevant data from a patient record database of the Hong Kong Hospital Authority. The study included male patients who were on monotherapy with long-acting alpha-1 adrenoreceptor blockers (AARBs) for LUTS between 2021 and 2022. Those with a history of urolithiasis or prostate cancer in the past five years or ROU in the past year were excluded.
The patients were divided into two groups: the COVID-19 group, consisting of those who had tested positive for SARS-CoV-2 infection, and the control group, consisting of those who did not have a positive polymerase chain reaction (PCR) test for SARS-CoV-2. The study outcomes included the incidence of BPH complications such as UTIs, bacteriuria, hematuria, and ROU, as well as the use of a 5-alpha reductase inhibitor (5ARI) as a combination therapy for LUTS.
After propensity score matching, the data of 17,986 individuals were analyzed, with each group consisting of 8,993 subjects. The study found significant differences in the incidence of BPH complications between the COVID-19 and control groups. The COVID-19 group had a higher incidence of ROU, hematuria, bacteriuria, and use of 5ARI.
The incidence of BPH complications was significantly higher in most age groups, except for younger age groups. There were notable differences in the incidence of bacteriuria and ROU in individuals aged 50 and above, as well as UTI incidence and 5ARI use in individuals aged 60 and above. The severity of COVID-19 did not affect the incidence of ROU, hematuria, or 5ARI use.
Interestingly, patients with asymptomatic or mild COVID-19 had a lower incidence of bacteriuria and UTI compared to those with more severe cases. Sub-group analyses also revealed that the incidence of hematuria remained higher in patients who were not on heparin therapy, and the incidence of bacteriuria and UTI remained higher after excluding patients prescribed steroids.
In conclusion, the study found a strong positive correlation between SARS-CoV-2 infection and an increased incidence of BPH complications in males with LUTS. This suggests that COVID-19 can have significant urological manifestations, and it is essential for urologists and clinicians to be aware of this additional burden. Older patients were found to be at a significantly higher risk of developing BPH complications. Furthermore, these urological manifestations can occur even in patients with mild or asymptomatic COVID-19. Further research is needed to fully understand the relationship between COVID-19 and BPH complications, and to explore potential preventive and therapeutic strategies.
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it