Researchers at the Technion’s Ruth and Bruce Rappaport Faculty of Medicine and the Rappaport Family Institute for Research in the Medical Sciences have made a significant breakthrough in the realm of immunotherapy. Their latest discovery revolves around a subset of blood cells that have the ability to forecast the success of immunotherapy treatments. This breakthrough is poised to revolutionize the process of matching patients with the most effective immunotherapy treatments, thereby enhancing treatment outcomes.
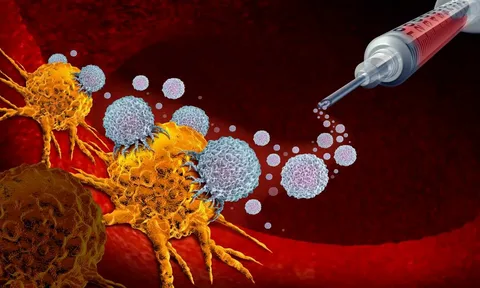
Immunotherapy stands out as a groundbreaking approach in cancer treatment, harnessing the body’s natural immune system to combat cancer cells with precision and efficacy. The challenge lies in the fact that cancerous tumors often evade detection by the immune system, undermining the body’s ability to eliminate them. Immunotherapy seeks to bolster the immune system’s capacity to recognize cancer cells as threats and unleash its full potential in combating the disease.
While immunotherapy has shown remarkable success in treating cancer, its efficacy is currently limited to approximately 40% of patients. This underscores the importance of delving into the biological responses to these treatments and pinpointing biomarkers that can forecast the treatment’s effectiveness.
Biomarkers play a pivotal role in personalized medicine, enabling healthcare providers to tailor treatment strategies according to individual patients’ needs and medical profiles. Although biomarkers are already utilized in immunotherapy, they are typically acquired through invasive biopsy procedures, which pose risks to patients and may not always accurately reflect the patient’s immune profile. Hence, there is a pressing need to explore alternative methods for predicting patients’ responses to immunotherapy.
The Technion researchers focused on antibody-based immunotherapy and identified biomarkers within the bloodstream that can anticipate a patient’s reaction to the treatment. Notably, these biomarkers eliminate the necessity of tumor biopsies, which can be invasive and hazardous to patients. The research unveiled the significance of a protein named STING, which triggers the immune system and is prominently active in cancer cells responsive to immunotherapy. This protein leads to the production of interferon protein, stimulating the differentiation of neutrophils into a specific subtype expressing the Ly6Ehi protein.
These specialized neutrophils play a crucial role in activating the immune system against cancerous tumors, potentially enhancing the effectiveness of immunotherapy. By assessing the levels of Ly6Ehi neutrophils in a patient’s blood, healthcare providers can efficiently gauge the patient’s response to immunotherapy treatment. The researchers corroborated their findings through preclinical investigations and clinical studies involving patients with lung cancer and melanoma, demonstrating the ability of neutrophils to accurately forecast immunotherapy responses in humans.
The technology developed by Prof. Yuval Shaked’s team has been patented and is currently undergoing a technology transfer process with the company OncoHost for further advancement. Prof. Shaked emphasizes that the technology can be seamlessly integrated with the widely available flow cytometry device, which is prevalent in hospitals and approved by regulatory bodies. This innovative approach holds tremendous promise in enhancing the efficacy of immunotherapy treatments and improving patient outcomes in the fight against cancer.
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it