What is a Spirometer?
A spirometer is a medical device used to measure lung capacity and performance. It is primarily used to diagnose and monitor conditions that affect breathing such as asthma, chronic obstructive pulmonary disease (COPD), cystic fibrosis, and COVID-19. During a spirometry test, the patient breathes into the mouthpiece of the spirometer which measures how much air they breathe in and out and how fast they can blow air out. Let’s deep dive into how a spirometer works and what it can tell us about our lung health.
How Does a Spirometer Work?
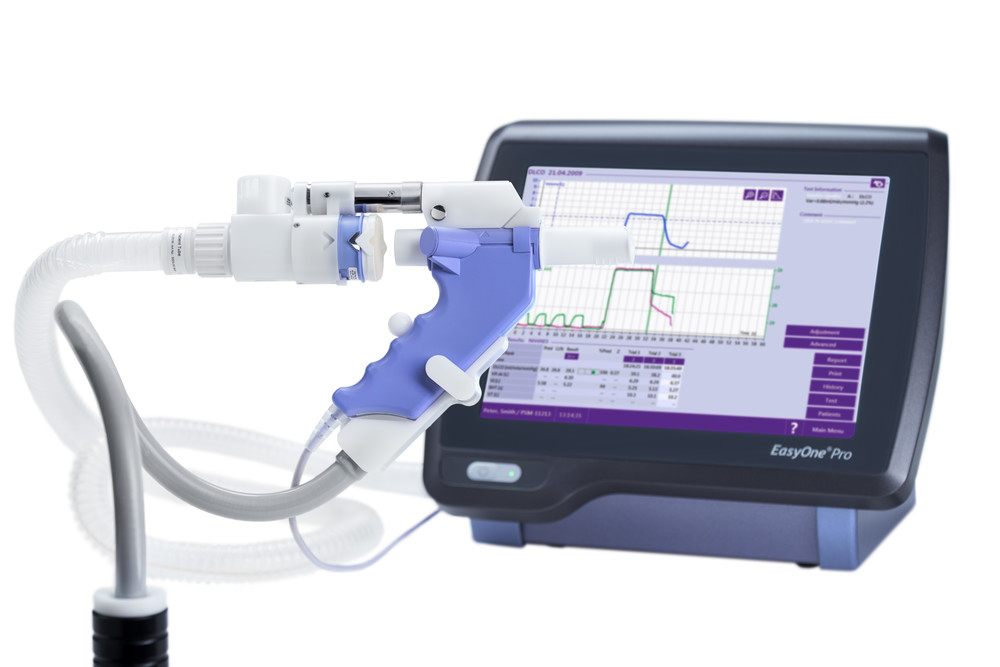
A spirometer consists of a mouthpiece attached to a series of tubes, valves, and a measuring device that records airflow. When a patient breathes into the mouthpiece, their exhaled breath travels through the apparatus. Most modern spirometers use sophisticated sensors and computer processing to convert airflow data into lung volume and flow rate measurements.
During a typical Spirometry test, the patient sits as still as possible and places the mouthpiece in their mouth, sealing their lips tightly around it. On the tester’s cue, they take a deep breath in and exhale as forcefully and quickly as possible until no more air can be expelled. This single forceful exhalation is called a forced expiratory maneuver (FEM). The spirometer measures parameters like Forced Vital Capacity (FVC), Forced Expiratory Volume in 1 second (FEV1), and the FEV1/FVC ratio.
Types of Spirometers
There are different types of spirometers used for various purposes:
– Desktop Spirometers: More sophisticated devices used in hospitals, clinics, and doctors’ offices. They provide printouts of lung function parameters and graphs.
– Handheld Spirometers: Portable devices preferred for home monitoring. They are smaller, easier to use and more affordable than desktop models.
– Waterless Spirometers: Uses sophisticated sensors instead of the displacement of water methodology of standard spirometers. More hygienic and easier to clean.
– Peak Flow Meters: Measures peak expiratory flow rate which reflects airflow limitation specifically in asthma. Easier to use than full spirometers.
What Can Spirometry Tests Tell Us?
Spirometry is invaluable for both diagnosing and monitoring respiratory diseases and conditions. Abnormal lung function values as compared to predicted norms can indicate various underlying pathologies. Some key insights provided:
– Obstructive vs Restrictive Lung Disease: Low FEV1/FVC ratio suggests obstruction like asthma; low FVC suggests restriction as in fibrosis.
– Asthma Diagnosis and Severity: Low FEV1 and FEV1/FVC in someone with asthma symptoms confirms diagnosis. Follow-up tests track response to treatment.
– COPD Diagnosis and Staging: Spirometry is essential to diagnose COPD and determine severity based on degree of airflow limitation.
– Post-COVID Lung Damage: Useful for tracking long-term respiratory impacts even after clinical recovery from COVID-19.
– Pre-operative Risk Assessment: Detects hidden lung conditions pre-surgery to optimize procedure planning and reduce risks.
– Cystic Fibrosis Monitoring: Tracks progression and response to treatment over time in people with cystic fibrosis.
The gold standard for measuring lung function, spirometry provides critically important objective data to both diagnose respiratory diseases early and guide effective ongoing treatment.
Spirometry – Considerations and Best Practices
There are several factors that need to be considered for reliable, consistent spirometry tests.
Patient Factors: The patient should not smoke, eat, or exercise heavily for at least 30 minutes before the test. They must understand instructions and give their full effort during FEMs.
Equipment Calibration: Spirometers need regular calibration checks to ensure accurate measurements. This may involve using a 3-liter syringe or mechanical pumps.
Test Technique: The technician should demonstrate FEMs, monitor for proper seal, encourage full exhalation and repeat tests as needed. Tests with poor quality should be discarded.
Test Interpretation: Lung function z-scores based on age, height, sex, ethnicity provide the most relevant comparisons versus raw numbers alone. Trends over time also inform about disease progression or treatment response.
Quality Assurance: Participation in external quality assurance programs helps address variability in technique and equipment among different testing sites for uniform application of spirometry.
Spirometry is a simple yet powerful test central to respiratory medicine. By objectively quantifying lung volumes and flows, it acts as a window into underlying lung pathology. When performed to standardized procedures and guidelines with proper equipment, calibration and quality checks, spirometry testing provides invaluable insights to diagnose, treat and monitor diverse respiratory conditions. It remains one of the most useful diagnostic pulmonary function tests available to both clinicians and patients.
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it