While the majority of parents understand the importance of vaccinating their children against potentially deadly diseases, some remain hesitant about certain vaccines. One such vaccine is the inactivated poliovirus vaccine (IPV) which protects against the polio virus. This article aims to provide information about IPV vaccines and highlight their critical importance.
What is Polio?
Polio, also known as poliomyelitis, is a highly infectious disease caused by the poliovirus. It mainly affects children under five years of age. The poliovirus spreads from person to person and can invade an infected person’s brain and spinal cord, causing paralysis. Up to 70% of infections cause no symptoms at all. About 1-5% of infections cause temporary flu-like symptoms such as sore throat, fever, tiredness, nausea, headache and stomach pain. A small percentage (less than 1%) of polio infections can result in permanent paralysis that is often life-threatening when the respiratory muscles are affected. There is no cure for polio, making prevention through vaccination one of the most effective tools.
History of Polio Vaccines
In the 1940s and 1950s, before polio vaccines were available, polio outbreaks caused widespread fear in industrialized countries. Mass polio outbreaks caused thousands of deaths and permanent disabilities each year due to paralysis and respiratory failure. In 1952 alone, nearly 58,000 cases of paralytic polio were reported in the United States.
To combat this, in 1955 Dr. Jonas Salk developed the first effective polio vaccine, also known as the inactivated poliovirus vaccine (IPV). It changed the course of history by containing three separate inactive poliovirus strains grown in monkey kidney tissue cultures. This vaccine required multiple doses to achieve immunity. A more user-friendly live attenuated oral polio vaccine (OPV) was later developed by Dr. Albert Sabin in 1961 which required fewer doses.
Global Polio Eradication Initiative
In 1988, the World Health Assembly launched the Global Polio Eradication Initiative (GPEI) with the goal of ending polio worldwide. A significant reduction in polio cases was seen as a result of vaccination efforts. However, some countries continued to experience outbreaks due to gaps in vaccination coverage, which allowed the virus to spread.
To interrupt wild poliovirus transmission, in April 2016 the World Health Organization (WHO) recommended all countries switch from trivalent OPV to bivalent OPV excluding the type 2 component due to rare cases of paralysis from vaccine-derived poliovirus. They also recommended countries using IPV alone or sequential IPV-OPV schedules. As a result of these actions, wild poliovirus cases have declined dramatically over 99.9% since 1988.
IPV vs OPV
While both IPV Vaccines and OPV provide excellent protection against polio, they work in slightly different ways:
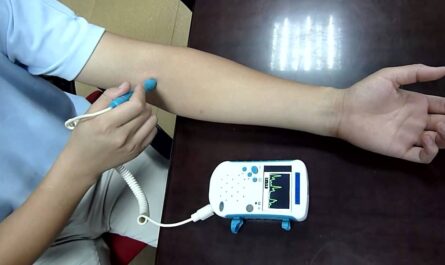
– IPV uses inactivated (killed) poliovirus strains that cannot cause polio but can still train the body to recognize and fight the virus. It is given as an injection in the leg or arm muscle. IPV provides excellent protection against paralysis to the vaccine recipient. However, it does not prevent infection or transmission to others.
– OPV uses live attenuated (weakened) poliovirus strains that can still replicate a little in the gut and induce immunity there while being unable to cause paralysis. It is given orally as drops. OPV provides greater gut immunity that also prevents infection and transmission to community levels. However, in very rare cases, the live attenuated virus in OPV can mutate and cause paralysis in vaccine recipients or their close contacts.
Due to these differences, WHO recommends countries use IPV for routine vaccination along with at least one dose of OPV to boost intestinal immunity during vaccination campaigns in polio-endemic regions or after outbreaks. High IPV coverage prevents polio cases while periodic OPV maintains immunity levels in communities needed to stop virus transmission.
Herd Immunity and its Importance
For a vaccine to be truly effective, a high level of herd immunity must be achieved through widespread vaccination. Herd immunity occurs when a large portion of a community (the herd) becomes immune to a disease, making the spread of disease from person to person unlikely. Even individuals not vaccinated (such as newborns or those with weakened immunity) are offered some protection because the disease has little opportunity to spread within the community. For polio, it is estimated that ≥80% of the population need immunity from vaccination to develop sufficient herd immunity to interrupt polio transmission.
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it