Causes and Risk Factors of COPD
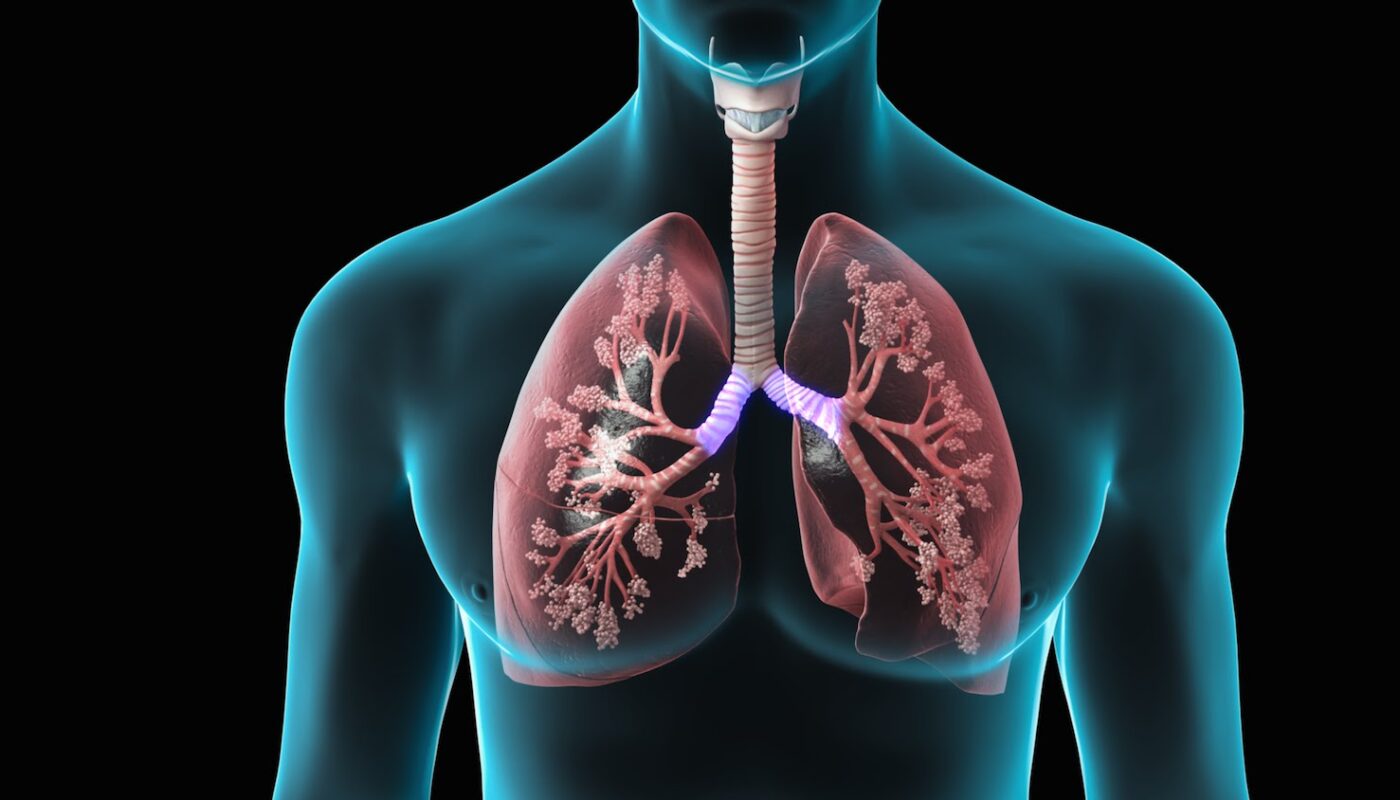
Chronic Obstructive Pulmonary Disease, commonly known as COPD, is a lung disease characterized by long-term breathing problems and poor airflow. The main causes of COPD are long-term exposure to irritating gases or particulate matter, most often from cigarette smoke. Other risk factors include genetics, age, air pollution and previous lung infections. COPD develops slowly over many years due to damage caused by risk factors to the airways and lung tissues. This damage is usually permanent and progressive, making breathing more and more difficult over time.
The primary cause of Chronic Obstructive Pulmonary Disease (COPD) Treatment is tobacco smoking. Cigarette, cigar and pipe smoke contain chemicals like tar and toxic gases that damage lung tissue when inhaled. The risk is proportional to the amount smoked over the years. Genetic factors also contribute, especially for those with alpha-1-antitrypsin deficiency, a condition which leads to lower levels of a protein that protects the lungs. Age is a risk factor since lung capacity naturally declines as we grow older. Long-term exposure to air pollutants in the indoor or outdoor environment can increase the likelihood of COPD as well. Previous lung infections like tuberculosis may also play a role.
Symptoms of COPD
The main symptoms of COPD are breathing difficulties, especially breathlessness or shortness of breath during activities. People often describe breathing issues as feeling like they cannot get enough air. Other symptoms may include a chronic cough with mucus, wheezing, chest tightness and frequent respiratory infections like bronchitis. As COPD progresses, sufferers may experience chronic tiredness, lack of energy and unintended weight loss. Some also experience episodes of acute worsening of symptoms known as exacerbations or flare-ups. During exacerbations, there may be increased cough, breathlessness and sputum production.
COPD Diagnosis and Treatment Options
COPD is diagnosed through a medical history, exams of the lungs and airways, and pulmonary function tests. Spirometry is a common test used to measure how much air the lungs can hold and how fast it can be expelled. The results are compared to normal limits to diagnose COPD and determine its severity stage which helps establish a treatment plan.
Treatment focuses on reducing symptoms, preventing and treating complications, and improving quality of life. The main options are as follows:
Bronchodilators: These medications work to relax and open airways by blocking chemical messengers that cause constriction. Short-acting inhalers are used as needed for relief while long-acting inhalers are prescribed every day to prevent symptoms.
Inhaled Corticosteroids: For patients with more severe disease, anti-inflammatory corticosteroids prevent exacerbations when used along with bronchodilators. They are delivered directly to the lungs through inhalers or nebulizers.
Oxygen Therapy: For those with severe lung damage and low oxygen levels in the blood, supplemental oxygen used for extended periods helps improve heart and lung function. Oxygen can be delivered via portable liquid or gas cylinders, oxygen concentrators or through nasal cannulas.
Pulmonary Rehabilitation: This involves exercise training and education to help optimize physical and emotional well-being. Breathing retraining teaches techniques to make activities of daily living easier. Nutritional counseling addresses weight management.
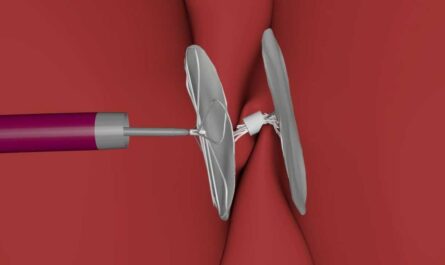
Bronchoscopic Procedures: Advanced treatments like lung volume reduction surgery or bronchoscopic lung volume reduction may provide benefits for selected COPD patients.
Vaccinations: Annual flu shots and one-time pneumococcal vaccines help prevent infections associated with exacerbations.
Lifestyle Changes: Quitting smoking, avoiding pollutants and managing medical conditions like asthma are important complementary steps to treatment. Maintaining a healthy weight and diet also supports lung health.
Surgery may be done in certain cases to treat complications like emphysema with lung volume reduction or lung transplantation for end-stage disease. The treatment approach will depend on the person’s specific symptoms, lung function test results and disease progression over time so periodic evaluation is important. An effective self-management plan matches individual needs to medications and therapy. Overall the goals are optimizing lung health, relieving symptoms and improving quality of life.
Adjusting to Life with COPD
Living with Chronic Obstructive Pulmonary Disease (COPD) Treatment requires ongoing adjustment both physically and emotionally. It is important to pace activities, rest when needed and prioritize good self-care. Home oxygen and portable oxygen concentrators help extend mobility within limits. Assistive equipment like shower stools, raised toilet seats and grab bars provide needed support. Joining a pulmonary rehabilitation or COPD support group allows social connection and education from peers experiencing similar challenges.
The emotional aspects of a chronic lung disease should not be ignored either. COPD prognosis varies but a proper treatment plan managed jointly with physicians aims to control symptoms and slow progression for overall wellness. Positive thinking and focusing on abilities instead of losses contributes to better coping. Family support helps reduce isolation, stress and depression. With coordinated medical treatment, healthy living adjustments often allow patients to participate in meaningful activities and maintain good quality of life for years despite lung damage.
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it