Perfusion is the process of circulating blood or other fluids through the blood vessels or lymphatics of an organ or tissue, typically to preserve cell function. Perfusion systems are machines that are used to perfuse organs outside the body, usually for organ transplantation. They help deliver oxygen, nutrients and remove carbon dioxide and waste from the organ being transplanted to keep it alive until it can be implanted into the recipient.
History of Perfusion Systems
The first successful organ perfusion was achieved in the 1930s when a dog kidney was preserved outside the body using a saline solution. This paved the way for further research into organ preservation techniques. In the 1950s, researchers developed techniques to perfuse organs with blood or various solutions instead of just saline. One of the major breakthroughs was the development of the Belzer UW (University of Wisconsin) solution in the 1980s. This hypothermic preservation solution helped significantly increase safe ischemic times for organs removed for transplantation.
Through the 1990s and 2000s, Perfusion Systems became more advanced with computer controlled pumps, oxygenators, heat exchangers and monitoring equipment. Today’s state of the art perfusion machines can closely mimic the conditions inside the body to keep donated organs protected, nourished and functioning until transplant. This has helped address the chronic shortage of donor organs worldwide.
Components and Functions of a Modern Perfusion System
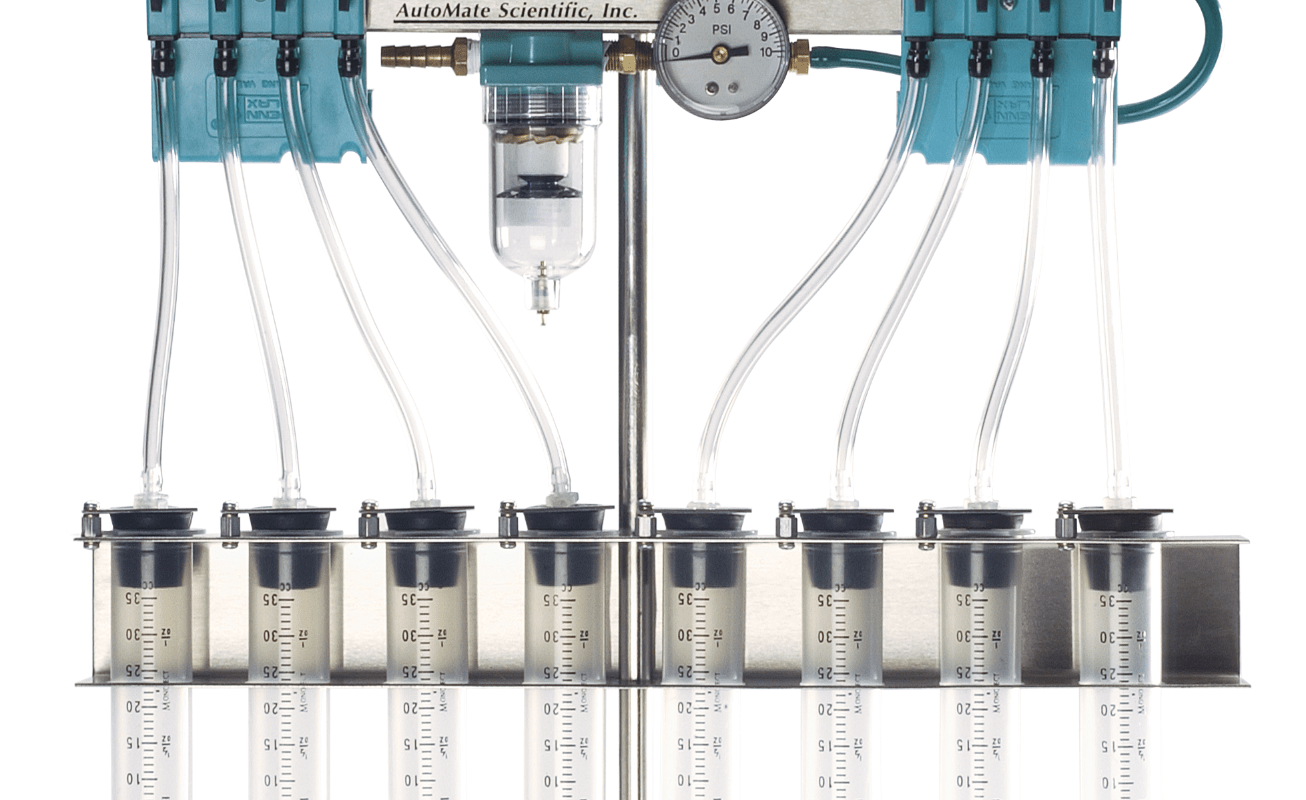
A typical modern organ perfusion system consists of the following key components:
– Pumps: Peristaltic or centrifugal pumps carefully circulate the perfusate through the organ at physiological pressures and flow rates.
– Reservoir: A storage container that holds the perfusate solution, usually an updated version of the UW solution.
– Oxygenator: Delivers oxygen to the perfusate and removes carbon dioxide, mimicking lung function. Most modern oxygenators use hollow fiber membranes for gas exchange.
– Heat Exchanger: Maintains the perfusate and organ at the desired temperature, usually between 34-37°C depending on the organ. This is crucial for organ viability.
– Filters: Removes cellular debris and metabolic wastes from the perfusate as it circulates through the organ. Different sized filters may be used.
– Sensors and Monitoring: Equipment to continuously track pH, pO2, pCO2, temperature, pressure, flow and other parameters crucial for organ preservation. Alarms alert staff to any undesirable changes.
Organs Currently Perfused and Areas of Research
Currently, the main organs that can be perfused outside the body include:
– Kidneys: Perfusion of deceased donor kidneys is now standard practice before transplantation to assess quality and restore function.
– Livers: Several centers worldwide are now practicing limited periods of normothermic perfusion for deceased donor livers prior to transplantation.
– Hearts: Some preliminary research involves perfusing donor hearts under working conditions prior to transplantation but this is still largely experimental.
– Lungs: Hypothermic perfusion is being explored but airless perfusion under physiologic working conditions presents unique technical challenges.
Areas of active research include development of normothermic perfusion techniques, adding immune cells to perfusate, assessment of novel preservation solutions, and using machine perfusion to evaluate marginal or extended criteria organs. Perfusion bio-markers and functional assessments are also being investigated to better predict post transplant organ function and survival. Long term machine perfusion is a focus to allow transportation of organs over longer distances.
Benefits of Perfusion
The major benefits of organ perfusion prior to transplantation include:
– Prolongs safe ischemic time: Perfusion protects organs in the relatively ischemia-free environment outside the body, allowing transport over greater distances between donor and recipient hospitals.
– Assesses organ quality: Parameters such as flow, resistance, biomarkers can help evaluate suitable organs and detect problems not evident with static cold storage.
– Restores organ function: Flushout of metabolic wastes and re-introduction of oxygen and nutrients to the perfused organ can improve function from suboptimal donors.
– Treatment of organs: Opportunity to treat organs with medications, change preservation solutions to reverse cold ischemia damage before implantation.
– Research platform: Perfused organs provide a unique human model outside the body to study preservation techniques, viability biomarkers and new treatments.
Challenges and Future Perspectives
Despite significant advances over past decades, challenges remain in perfusing all organ types and standardizing techniques across transplant programs. Specialized expertise, additional costs and logistical complexities also need to be addressed for wider clinical adoption. With growing organ demand-supply gaps, machine perfusion offers great promise but further innovation is still needed. Areas ripe for development include perfusing vascuarly fragile organs like lungs, use of autologous carriers for organ transportation and establishing normothermic regional sharing networks. Successful research in these areas could help expand both the quantity and quality of organs available for patients awaiting lifesaving transplants.
In summary, organ perfusion plays a vital role in transplantation by enabling longer preservation outside the body, assessing organ quality and improving donor organ function. With further progress, perfusion technology coupled with expanded donor criteria may help significantly increase the number of organs transplanted worldwide in future.
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it